Why Is Serotonin-2A Brain Receptor Binding Reduced in Depression?
New scientific work continues to show a complicated relationship between depression and the serotonin system
This is a discussion of the article: Chapman GE, Turner G, Noar AP, Barba T, Zafar R, McCutcheon RA, Erritzoe D. Cortical 5-HT2A receptors in depression and suicide: a systematic review and meta-analysis of in vivo and post-mortem imaging studies. Molecular Psychiatry. 2025.
Epistemic status: preliminary and evolving scientific understanding
As far as we know, clinical depression is not fundamentally a result of serotonin deficiency or serotonin abnormalities of other sorts; however, available research continues to show the involvement of the serotonin system in depressed mood in a complex manner. The latest in this line of work is a paper by George E. Chapman and colleagues in Molecular Psychiatry that is a systematic review and meta-analysis of human studies looking at a particular type of serotonin receptor, the 5-HT2A receptor, in the brain cortex.
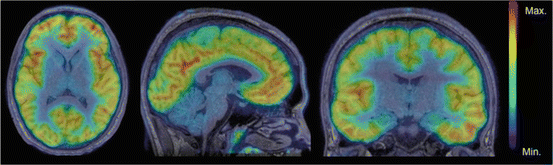
Among serotonin receptors, 5-HT2A, is the most abundant in the human cortex, especially in prefrontal and cingulate regions tied to mood and cognition. It is influenced indirectly by traditional antidepressants, acted-on directly by several add-on medications (such as second-generation antipsychotics) and all classical psychedelics act primarily on this receptor. The presence and density of these receptors can be quantified in living humans with brain imaging using established radiotracers, and a number of research trials have investigated it in the past, with some mixed results. (In case you are wondering, the 2022 Moncrieff et al. umbrella review did not look at 5-HT2A.)
Authors of the present paper reviewed and combined evidence from brain-imaging studies (PET and SPECT) and post-mortem radioligand studies that measure how strongly tracers bind to cortical 5-HT2A serotonin receptors (5-HT2ARs) in people with major depression and in individuals who died by suicide. From each study, they extracted receptor-binding data and pooled results using random-effects meta-analysis. 31 studies contributed data from 556 people with major depression or who died by suicide and 526 healthy controls. They focused on patients who were unmedicated at the time of the study, from at least one week to never having taken them.
They found the following:
In living MDD patients who were actively depressed and were off antidepressants at the time of the study, cortical 5-HT2A receptor binding was lower than in controls in several brain areas (frontal, prefrontal, cingulate, anterior cingulate cortex, and temporal cortex). The associations were generally of a medium size (effect sizes ranged from g = –0.40 to –0.57).
In the frontal and cingulate regions of the brain, lower binding tracked with more severe depression at baseline.
Among never-medicated patients, study-level results also pointed to lower binding than controls; an exploratory meta-analysis showed this reached significance in the anterior cingulate.
Most PET/SPECT studies were good or fair quality.
Post-mortem findings were mostly null and study quality varied.
I am going to focus here on the interpretation of the primary finding that 5-HT2AR binding is reduced in depression in several brain regions in living humans. What does this mean, and why is this happening?
At face value, the finding challenges the straightforward idea that serotonin transmission is reduced in depression, because if that were the case, we would expect 5-HT2AR, which are post-synaptic, to be up-regulated as a compensatory response. The other straightforward explanation would be that the reduced binding is entirely due to medication effects; since antidepressants such as SSRIs boost serotonin in the synapse, the body compensates by reducing the number of serotonin receptors. This would be expected and also rather uninteresting, but the results of the meta-analysis suggest that medication is only part of the explanation, and a more creative interpretation is required. Depression itself appears to be linked to lower cortical 5-HT2ARs binding, such that the binding differences increase with the course of illness and with treatment.
(For lay readers: Neurons that communicate meet at a tiny gap called a synapse. The sending side, the presynaptic neuron, releases chemical messengers, such as serotonin, into that gap. The receiving side, the post-synaptic neuron, has receptors waiting to catch the message. 5-HT2A receptors sit mainly on the membrane of the receiving neuron. Post-synaptic receptors can increase or decrease in density or activity based on what’s happening in the synapse; if there is too much serotonin being released, for example, over time the brain can compensate for it by producing less serotonin receptors.)