Biotypes in Depression and Anxiety — At Long Last, Progress
Celebrating groundbreaking work by Leanne Williams & colleagues
A team of researchers led by senior author Leanne Williams has recently reported in Nature Medicine that they have identified distinct and clinically relevant profiles of connectivity and activity of brain circuits in individuals with depression and anxiety disorders. This is based on data from functional magnetic resonance imaging (fMRI) with a focus on six brain circuits where were believed to be implicated in depression and anxiety based on prior research. The distinct profiles (“biotypes”) also show differences with regards to symptoms, behavioral performance on various tasks, and response to medications and behavioral therapy. These findings are a milestone in the pursuit of precision psychiatry.
Some readers may be understandably skeptical… why should this report be any different from so many other biomarker associations whose discoveries were announced with much fanfare but which didn’t pan out, were quickly forgotten, and had little scientific impact. What I find truly exciting here are not the statistically significant empirical associations but rather the theoretical taxonomy based on decades of neuroscientific research which guided this research project and which has been validated by these results. The findings make mechanistic sense and cannot be treated as unanticipated chance findings in a fishing expedition.
Let me explain.
The 2024 Nature Medicine paper is the product of a decades-long research program to better understand the neural circuit architecture of psychopathology, and this background is vital to appreciating its significance. In a 2016 paper for Lancet Psychiatry, Williams suggested a neural circuit taxonomy for depression and anxiety based on a review of literature. I was a psychiatry resident when the paper was published and I remember reading it with excitement. The memorable figures from that article have stayed with me ever since.
Findings from a large number of fMRI studies of depression seem to converge on changes that involve (at least) 6 large-scale circuits.
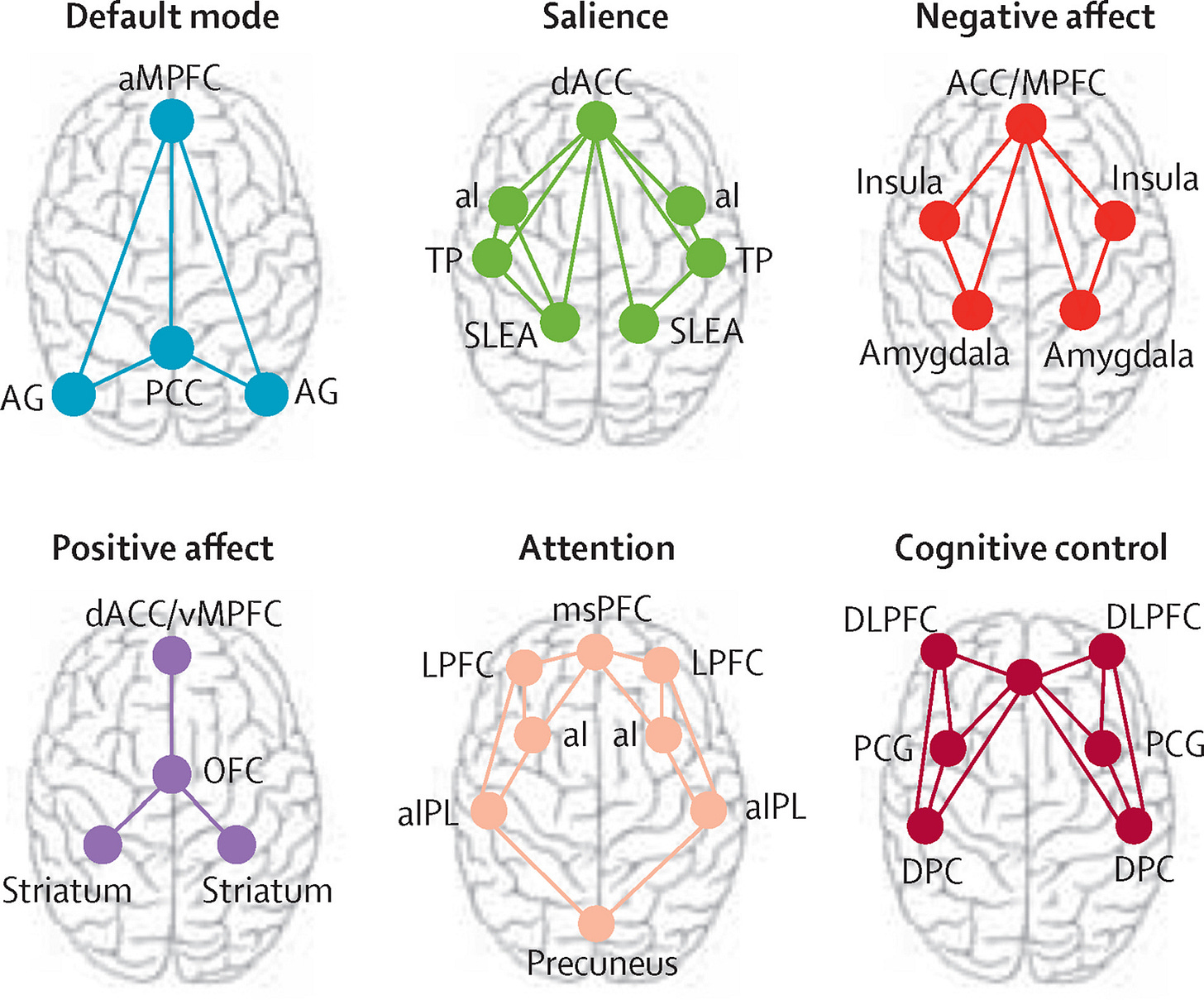
Default mode network is observed to be active when the individual is at rest, not engaged in any particular mental task, or when people are reflecting on their own spontaneously generated thoughts.
Salience circuit is involved in the detection of bodily and environment changes and signals the need for mental effort in response to those changes
Negative affect circuit is activated by stimuli, such as facial expressions, that signal potential threat, and regulates emotional responses such as fear and anger
Positive affect circuit is preferentially involved in sensitivity to and anticipation of rewards
Attention circuit is implicated in alertness and sustained attention. It works in coordination with the default mode network in back and forth between a state of rest and a state of being engaged in tasks.
Cognitive control circuit is involved in working memory, selective attention, and cognitive flexibility.
(These are rather simplistic descriptions of the roles of these brain circuits. Think of the brain circuits as being differentially involved in these processes, such that there are multiple brain circuits involved for any given behavioral phenomenon and any given brain circuit plays a role in multiple behavioral phenomena.)
Williams proposed in the 2016 paper that there are at least 8 distinct ways that these 6 brain circuits could get disrupted via alterations in connections between parts of the circuit (hyper- or hypo-connectivity) and activity of the circuits (hyper- or hypo-activity). She called them “biotypes,” and hypothesized that different patterns of alterations reflect different clinical features and possibly different responses to treatment.
The following list is copied verbatim from a table by Williams (2022) in Psychiatric News summarizing the hypothesized biotypes, the circuits involved, and salient clinical characteristics:
Rumination — Default mode connectivity — Tendency to repeatedly worry and focus inwardly on negative thoughts
Anxious avoidance — Salience network connectivity — States of anxious arousal and apprehension, which commonly involve physical symptoms, prompt avoidance of anxiety-inducing stimuli and situations
Negative bias — Negative affect circuit response to mood-congruent stimuli — Excessive orientation to negative stimuli and a cycle of catastrophizing
Threat regulation — Negative affect circuit responsive to threat-related stimuli — Automatic fear reactions to actual or perceived threat that may be hard to switch off
Anhedonia — Positive affect circuit responsive to reward stimuli — Inability to take pleasure in activities that usually bring joy and provide a sense of purpose
Context insensitivity — Positive affect circuit responsive to context — Loss of motivation and disengagement even in otherwise motivating contexts, both positive and negative
Inattention — Fronto-parietal attention circuit — Difficulty concentrating and staying focusing
Cognitive dyscontrol — Cognitive control circuit engaged by tasks — Impairments in executive functions requiring inhibition
Over the years, research has also been conducted on how the functioning of various brain circuits is related to treatment responses, with some relevant findings summarized in this table.
The analysis by Tozzi et al. in the latest Nature Medicine paper was conducted using combined data from 4 trials (iSPOT-D, RAD, HCP-DES, and ENGAGE). These subjects (n = 801) represented the full spectrum of severity of depression and anxiety disorders. Healthy controls were used as a reference group for calculating brain circuit scores. Out of the 801 subjects, 250 completed RCTs of antidepressants for major depression (n = 164) or behavioral intervention for clinically substantial depressive symptoms and obesity (n = 86). Researchers had fMRI brain data from subjects at rest (task-free) and when they were engaged in different tasks designed to test their cognitive and emotional functioning (task-evoked).
Vast majority (95%) of subjects were not receiving antidepressant treatment at baseline. Researchers obtained 41 measures of activation and connectivity of 6 brain circuits of interest for each participant. Quantified circuit measures were expressed as standard deviation units from the mean of healthy controls, resulting in a “regional circuit score” for each individual. These scores were fed to a hierarchical clustering algorithm, and across multiple methods (used to ensure validity), a six cluster solution emerged as viable. The six resulting biotypes were distinguished by specific profiles of both task-free and task-evoked activity and/or connectivity, relative both to each other and to the healthy reference sample.

Notable features of each biotype are as follows.
Biotype DC+SC+AC — Hyperconnectivity of default mode, salience, and attention circuits
slowed behavioral responses in identifying sad faces and target stimuli in a sustained attention task
less errors in a cognitive control task
better response to behavioral treatment (Effect Size 0.61, 42% responders)
Biotype AC — Attention circuit hypoconnectivity
less severe tension symptoms
performance on tasks suggestive of reduced concentration with impulsivity
comparatively worse response to behavioral treatment (ES 0.59, 26% responders)
Biotype NSA+PA+ — Hyperactivity of negative affect and positive affect circuits
more severe anhedonia and ruminative brooding
Biotype CA+— Hyperactivation of the cognitive control circuit
more severe anhedonia, anxious arousal, negative bias, and threat dysregulation
deficits in executive function and sustained attention tasks
better response to venlafaxine (ES 0.43, 64% responders)
Biotype NTCC-CA-— Hypoactivation of cognitive control circuit and hypoconnectivity of negative affect circuit
less ruminative brooding (ES 0.9)
faster reaction times to sad faces (ES 0.67)
Biotype DXSXAXNXPXCX — Intact activation and connectivity
absence of prominent circuit alterations
These empirically-derived biotypes are congruent with the theoretical biotypes suggested earlier by Williams, and Supplementary Table 16 in the paper provides an instructive comparison. Biotype DC+SC+AC+, for example, is a combination of biotypes #1 (Rumination) and #2 (Anxious Avoidance).
NSA+PA+ is a combination of Williams’s #3 and #6; NTCC-CA- is a combination of #8 and #4, AC matches with #7, and CA+ matches with compensatory analogue of #8.
This suggests something important: the theoretical biotypes proposed by Williams may be more like fundamental profiles of circuit alterations that can empirically exist in actual patients in a variety of combinations and configurations.
What we should look for in future research is not an exact replication of the 6 biotypes reported in the Nature Medicine paper but whether future circuit dysfunction profiles can be similarly explained in terms of combinations of fundamental disruptions of circuit connectivity and activity. The optimal clustering solution for any given sample would depend on the particular composition and characteristics of that sample.
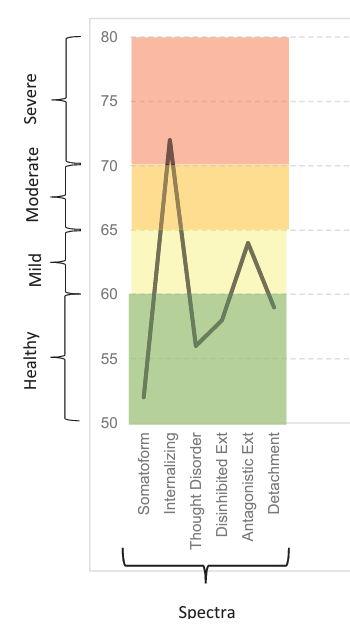
These empirically-derived “biotypes” can be misleading if we think of them as categorical boxes into which any particular person with depression and anxiety must fit. It is more accurate to think of each person as having a distinctive profile of circuit alterations, which can be visualized as:

This is a similar sort of shift in perspective from DSM/ICD to HiTOP, i.e. a shift from assigning a categorical diagnosis to creating a dimensional profile:
These empirically-derived “biotypes” can be misleading if we think of them as categorical boxes into which any particular person with depression and anxiety must fit. It is more accurate to think of each person as having a distinctive profile of circuit alterations.
Not only is circuit dysfunction dimensional, it is also transdiagnostic.
The biotypes cut across boundaries of DSM diagnoses, as we have anticipated for many years now:

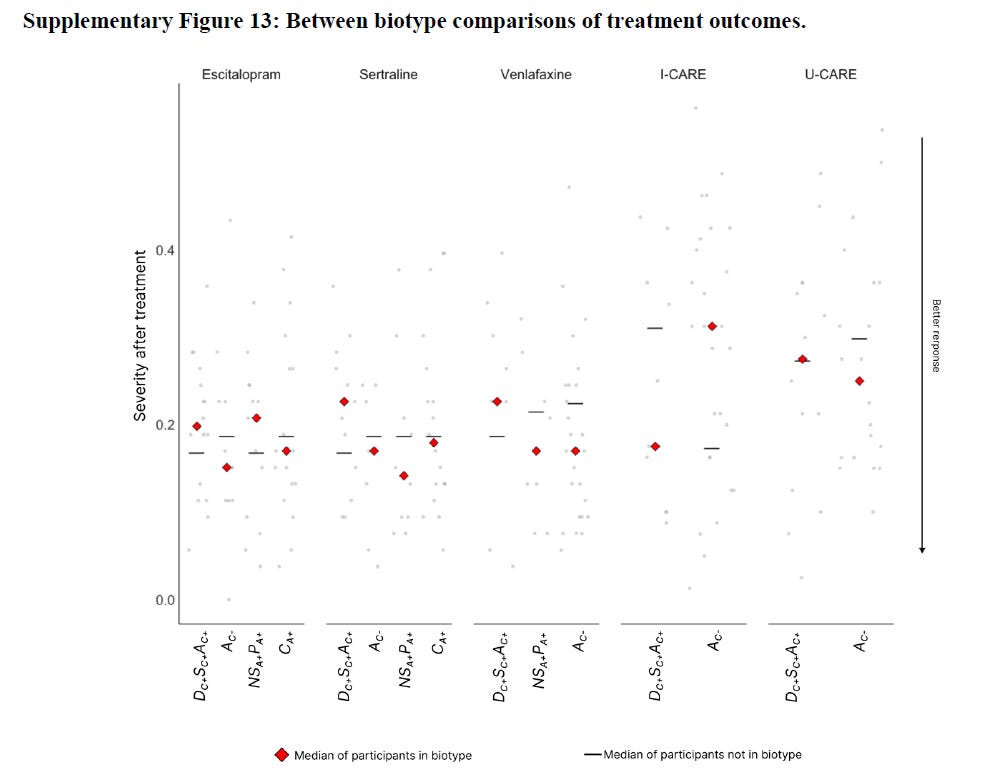
To make matters complicated and interesting, biotypes based on brain circuit scores are not the only valid way of biotyping. Researchers compared their results in the Nature Medicine paper to other approaches, e.g. using whole brain connectome rather than regional brain circuit scores. Brain circuit scores outperformed other approaches, but other approaches also yielded statistically significant associations among various metrics related to symptoms, behavioral tasks, and treatment response. For example, using an approach taken previously by Drysdale et al. 2017 yielded significant associations for both sertraline and venlafaxine rather than just venlafaxine as above (see supplementary tables 13 and 14).
This suggests that just as there is flexibility in carving the phenomenological space of psychopathology such that multiple ‘correct’ solutions are possible with respective advantages and disadvantages, it appears likely that the space of circuit dysfunction can be similarly classified in multiple ways and some solutions outperform others on metrics of interest to us.
The biotypes show statistically significant differences among symptom domains but the magnitude of the differences is modest. It is not possible to distinguish biotypes with any accuracy simply by looking at the symptom profile of a patient. The biotypes are indeed clinically distinct in the sense that they show differences that are statistically significant, but they are not distinct enough that we can rely on clinical characterization as a proxy. The messy overlap of clinical symptomatology will be obvious from this figure:
In contrast, differences in treatment responses, where present, are of comparatively greater magnitude and could be of genuine clinical value. This would, of course, require demonstration in prospective clinical trials designed to study the utility of treatment selection guided by fMRI biotypes. Despite the overall large sample, the number of subjects in any particular treatment arm in this study was still small, and with a larger sample, we may also have potentially seen statistically significant differences in response to sertraline and escitalopram.
An interesting question in my mind is whether treatment response is better guided by biotypes, as in this study, or whether we are better off focusing directly on the characteristics of alterations in individual circuits (as noted in the table by Song, Tozzi, & Williams, 2024 above).
And finally, it is important to say out loud that discovery of brain circuit biotypes does not collapse the multi-level (so-called bio-psycho-social) etiology of mental disorders into a simplistic model of biological dysfunction and causation. These profiles of brain circuit alterations are embedded within multi-level causal networks with criss-crossing physiological, experiential, and relational processes. There should be little doubt about that.
The work by Williams and her colleagues is a powerful demonstration that brain processes underlying psychopathology are not utterly incoherent. The neural architecture is at least partly discernible and it is clinically relevant. We are at the beginning of a new era of translational research. We may see an explosion of clinical trials based on fMRI biotypes. There are no simple, biological answers to be found in the form of disease entities akin to neurosyphilis when it comes to psychopathology, but there are some answers to be found in the form of dimensional and transdiagnostic associations with patterns of brain activity.
See also: